HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Translational Research Workshop Bridges Gap Between Bench Research and Clinic
 If you glance at a diagram of the continuum of translational research, the arrows point orderly to five phases — from basic research to improving population health. Rarely, however, is the business of discovery so neatly aligned. It takes unexpected twists and turns, as attendees at this week’s Children’s Hospital of Philadelphia Translational Research Workshop for Basic Scientists heard from experienced investigators who shared lessons that they’ve learned while pursuing their scientific endeavors.
If you glance at a diagram of the continuum of translational research, the arrows point orderly to five phases — from basic research to improving population health. Rarely, however, is the business of discovery so neatly aligned. It takes unexpected twists and turns, as attendees at this week’s Children’s Hospital of Philadelphia Translational Research Workshop for Basic Scientists heard from experienced investigators who shared lessons that they’ve learned while pursuing their scientific endeavors.
Twenty workshop participants, including junior faculty as well as postdocs and grad students, came from CHOP’s campus, local institutions, and science laboratories from across the U.S., including California, Texas, Boston, and Puerto Rico, for the intensive three-day educational program that introduced them to the latest methods and approaches in cutting-edge translational research at CHOP Research Institute.
One attendee joked that her reason for traveling so far to take part in the workshop was that, “I mainly work with mice, so I’m excited to see humans.”
Translational research is the process of turning observations in the lab, clinic, and community into interventions to improve the health of individuals and the public, from diagnostics and therapeutics, to medical procedures, to behavioral change. It’s easier to put into words than into practice.
“Translation may seem like an automatic part of research and medical practice, but in reality it’s a major stumbling block in science, medicine, and public health,” said the workshop’s host,Nancy B. Spinner, PhD, chief of the division of Genomic Diagnostics at CHOP and professor of Pathology and Genetics at the Perelman School of Medicine at the University of Pennsylvania.
The workshop, which was organized by the Institute’s Office of Postdoctoral Affairs, exposed attendees to unique aspects of CHOP’s scientific enterprise that are aimed at overcoming these obstacles. In a conference room at the Colket Translational Research Building, they listened to lectures given by a diverse group of presenters. Their varied backgrounds demonstrated how it often takes the convergence of a mix of disciplines to reach breakthroughs in translational research. The speakers covered a wide range of topics from the nuances of quality improvement science — a new field that is gaining attention — to how and why CHOP physician-scientists have spent a decade unraveling the genetic basis of congenital heart defects.
Alexion pharmaceuticals, a global biopharmaceutical company that focuses on rare diseases and orphan drugs, sponsored the workshop. Stephen Uden, MB, who leads research at Alexion, gave a presentation that described how new discovery ideas proceed through the drug and device development pipeline, from bench to market.
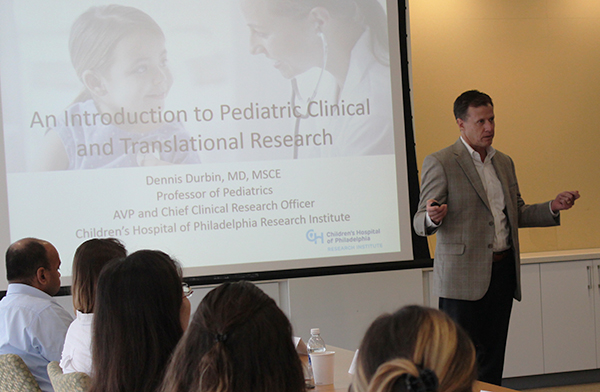 Dennis Durbin, MD, MSCE, assistant vice president and chief clinical research officer of the Research Institute, spoke about what is “under the hood” of a major pediatric research institution, which has a framework in place for clinical research practices through the Clinical Research Support Office.
Dennis Durbin, MD, MSCE, assistant vice president and chief clinical research officer of the Research Institute, spoke about what is “under the hood” of a major pediatric research institution, which has a framework in place for clinical research practices through the Clinical Research Support Office.
“One of the nice things about being a hospital-based research institute, is that we have a ‘bench to bedside’ concept,” Dr. Durbin said. “Close to everything we do should somehow be connected to advancing child health… At CHOP we’re supportive of our basic science program, but we also have a full spectrum of research going on here.”
Dr. Durbin described the 20 years that he devoted to population health research as a clinical epidemiologist interested in motor vehicle safety. The discoveries he made with his team at the Center for Injury Research and Prevention — along with other research stakeholders such as auto manufacturers, auto insurers, seatbelt manufacturers, and car seat makers — have saved 15,000 children’s lives over the last 15 years.
Behind the science success stories, attendees also heard how the presenters’ career paths revealed themselves, sometimes through good fortune and by being open to new opportunities. Dr. Spinner shared that she has an undergraduate degree in anthropology. Her passion to pursue graduate school and specialize in the field of genomics began when she traded in a college job scooping ice cream for a work study position in the lab of Jeffrey Hall, now a retired professor from Brandeis University, who shared the 2017 Nobel Prize in medicine for his research that revealed new insights about circadian rhythms, our bodies’ biological clock.
 Dr. Spinner recently celebrated her 25th anniversary at CHOP/Penn and called the campus a “fantastic place for me… Part of the reason I’ve been so thrilled to be here is we have basic science, an outstanding university, a medical school, and a nursing school. We have people from all walks of science, and over my career, I’ve collaborated with experts from many of these places.”
Dr. Spinner recently celebrated her 25th anniversary at CHOP/Penn and called the campus a “fantastic place for me… Part of the reason I’ve been so thrilled to be here is we have basic science, an outstanding university, a medical school, and a nursing school. We have people from all walks of science, and over my career, I’ve collaborated with experts from many of these places.”
The workshop group was invited to see some of these valuable resources firsthand. They took a hospital tour; visited its Center for Human Phenomic Science, which is the home base for many of the 600 clinical trials being conducted at CHOP; and met the staff at the Center for Autism Research.
They were introduced to the inner workings of CHOP’s Institutional Review Board (IRB), which is the hospital’s research ethics committee. Members of the IRB have expertise in scientific areas, the conduct of research, federal and state laws that govern research, CHOP policies, and the rights and welfare of study participants. Workshop attendees participated in a mock IRB session that gave them an interactive look at how investigators and reviewers work through potential sticking points before a clinical trial gets underway.
In a heartwarming presentation, attendees also heard the perspectives of a patient and her family who benefited from a novel drug that evolved from a translational research approach. In 2009, a team of CHOP oncologists, geneticists, and colleagues reported that they had identified a major familial neuroblastoma predisposition gene, called anaplastic lymphoma kinase gene (ALK). They developed robust scientific models that demonstrated it was an important drug target, which helped to gain the interest of a pharmaceutical company that supported a clinical trial to prove the safety and efficacy of a ALK inhibitor specially formulated for young children.
Edie Gilger, was diagnosed with the rare, inherited form of neuroblastoma, a cancer of the nerve tissue, at just 6 months old. With the help of the experimental drug offered in the clinical trial led by Yael Mossé, MD, a CHOP pediatric oncologist and physician-scientist specializing in neuroblastoma, Edie fought off the tumors growing in her spine and belly. Now 8-years-old, Edie’s scans at CHOP this week confirmed that she has remained cancer-free for 6 ½ years. Her mother, Emily Gilger, who was diagnosed with neuroblastoma about a year after Edie’s cancer went into remission, also was treated successfully at CHOP/Penn with a different version of an ALK inhibitor.
“Obviously, we owe our lives to things that are being done in the lab by people who take the time to do the research for these advanced studies that are saving hopefully many other children’s lives around the world,” Emily Gilger said.