HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Frontier Program Aims to Address Daunting Challenges of Heart Valve Disorders

With a multidisciplinary team of experts, the Pediatric Heart Valve Center aims to be a “one-stop shop” for patients with heart valve disease.
Heart valve disorders — congenital and acquired — are among the most common and severe forms of heart disease in children. Yet despite this prevalence, outcomes for these pediatric patients remain challenging because treatment options are limited.
To date, there are no available catheter-based solutions to improve valve regurgitation in babies. As for surgery, valve repair is particularly complex in newborns and infants. Of these tiny patients in whom prosthetic valve replacement may be possible, at least three additional open heart procedures will be necessary to upsize the valve as the child grows into adulthood. Among infants and young children requiring valve replacement therapies, one-year surgery mortality can often approach 20 percent.
Addressing these daunting challenges is Children’s Hospital of Philadelphia 2021 Frontier Program, the Center for Pediatric Heart Valve Disorders, a multidisciplinary collaboration with experts from across the Cardiac Center working in cardiac surgery, interventional cardiology, and cardiac imaging. Scientists and researchers will join them in a coordinated approach to treating valve diseases and expanding the existing knowledge of these complex conditions. By encompasses basic science, translational research, highly advanced imaging, innovative surgical alternatives, and access to current and emerging therapeutics not available nationally, the Pediatric Heart Valve Center aims to be a “one-stop shop” for patients with heart valve disease.
“With recent growing momentum of expertise across a continuum of discovery,” said Jonathan Chen, MD, the Center’s surgical director, “the CHOP Cardiac Center stands poised to establish the Pediatric Heart Valve Center as an unrivaled vanguard collective that will transfigure and transform the field of pediatric valve therapeutics.”
Meet the Team
Leading the Pediatric Heart Valve Center are Dr. Chen; Matthew Gillespie, MD, medical director of Interventional Cardiology; and Michael Quartermain, MD, medical director of cardiac noninvasive imaging. Other key members of the multidisciplinary team include Robert Levy, MD, who will take the helm of the basic science effort, while Matthew Jolley, MD, and Lindsay Rogers, MD, will continue to develop and work with advanced echocardiographic and three-dimensional imaging.
“The expertise and thought leadership from surgery, interventional cardiology, imaging, and basic science provides a unique and strong position for the Center to advance the field and truly make an impact,” said Dr. Chen, who is also chief of the Division of Cardiothoracic Surgery.
Pictures are Worth a Thousand Words
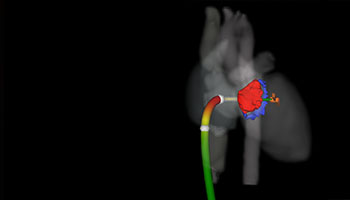
Simulated delivery of transcatheter clip-based therapy in CT image-derived patient specific model.
By integrating novel imaging platforms such as 3D echocardiography and virtual reality in surgical and transcatheter planning, the Center is looking to develop new approaches to treating valve disorders in children.
Take for instance, Dr. Jolley’s research. Described by Dr. Chen as a “true MVP in our field,” Dr. Jolley has an active laboratory that’s investigating the mechanisms of pediatric heart valve disease. One specific focus is to develop modeling techniques to see how transcatheter technologies can be applied within pediatric valve disease. Dr. Jolley’s work is leading to precision medicine in the field of cardiology as it pertains to understanding specific patients’ valvular heart pathology and possible interventions that can be developed or implemented to adjust these problems.
“We may be able to create 3D echocardiogram based models in real patients, and those models may be of clinical utility,” Dr. Jolley said in a recent CHOP Pediatric & Congenital Heart Talks video interview in which his 3D imaging and virtual reality research can be seen in action. “Ultimately, the integration of these technologies could significantly inform the way we manage and intervene upon children with valve disease.”
Minimally Invasive Techniques
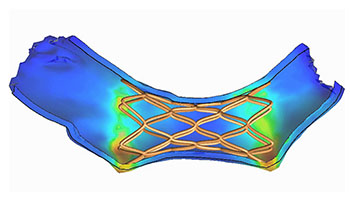
Finite element modeling of deployed self-expanding transcatheter valve in the pulmonary artery.
Lifesaving advancements have been made over the last decade in the use of transcatheter therapies, allowing an interventional cardiologist to repair and treat the heart, or surrounding areas, with the use of a catheter, a flexible hollow tube that threads through a blood vessel and into or near the heart. These less invasive procedures reduce the many risks associated with open heart surgery.
As medical director of the Cardiac Catheterization Lab at CHOP, this is Dr. Gillespie’s area of expertise. He is a lead investigator on several ongoing transcatheter valve clinical trials — a transcatheter pulmonary valve clinical study, and two multicenter studies (ALTERRA and COMPASSION S3) of congenital pulmonic valve dysfunction. He has a longstanding research interest in the development of novel transcatheter therapies for patients with congenital heart disease (CHD). With a published record of inventing and testing novel technologies in preclinical models of heart valve dysfunction, such as mitral, pulmonary, and tricuspid valve regurgitation, Dr. Gillespie has helped CHOP attain national prominence as a leader in transcatheter valve replacement therapies.
“Catheter-based therapies for heart valve dysfunction have expanded dramatically over the last 20 years,” Dr. Gillespie said. “Together with our imaging and surgical colleagues, we’re working in the CathLab to expand the use of minimally invasive technologies to treat pediatric and adult CHD patients suffering from heart valve disorders.”
The Need for Medical Therapeutics
CHOP’s director of Cardiology Research, Dr. Robert Levy and his team in the Levy Lab have been digging deep into the basic mechanisms and novel therapies for heart valve disease for decades. The pathophysiology of biomaterials used in medicine is one of his research interest areas, specifically investigating the failure mechanisms of biomaterials used in heart valves.
“The Achilles heel of implanting a tissue valve in any position is that it breaks down over time,” Dr. Chen said. “Children have a particularly accelerated rate of prosthetic valve calcification, causing the valve to stop working sometimes in less than five years. So for that reason, tissue valves are almost never used in children as a valve replacement technology.”
Help could soon be on the way though, as Dr. Levy is conducting the first preclinical studies of medications that may mitigate the progression of valve pathology in children. Two types of studies will be performed using blood samples from patients. One involves testing platelets, the small blood components involved in the formation of blood clots, for their response to medications that may limit platelet contributions to the progression of heart valve disease. The second study involves establishing cell cultures from patients’ blood samples, which will be used as disease models for valve disorders. Both types of studies represent a personalized medicine approach to assess each patient’s potential response to medications, but without the patients being directly administered drugs.
“Major advances in cardiac surgery over the past 60 years have led to the discovery, development, and successful use of prosthetic heart valves in children and adults,” Dr. Levy said, “as well as innovative cardiac valve repair procedures, for the treatment of heart valve disease. Nevertheless, the lack of any medical therapies or even therapeutic targets for heart valve disease represents a major unmet need that this new CHOP Frontier program will address.”