HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
Can Medication Improve Blood-Brain Barrier Function in 22q Deletion Syndrome?
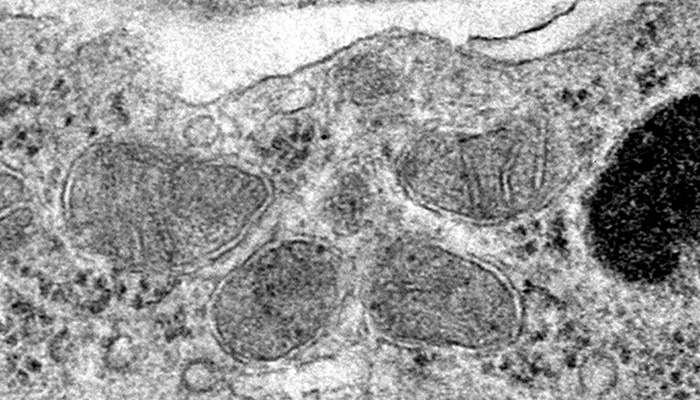
Electron microscopy imaging shows healthy mitochondria in brain endothelial cells from animal models of 22q.11.2 deletion syndrome that were treated with bezafibrate. (Credit: Courtesy of the Alvarez Lab)
The Findings
Researchers at Children's Hospital of Philadelphia and the University of Pennsylvania School of Veterinary Medicine found in a preclinical study that mitochondrial dysfunction in the blood-brain barrier may underlie neuropsychiatric symptoms in some patients with 22q11.2 (22q) deletion syndrome, a genetic disorder that affects many parts of the body.
The researchers showed that bezafibrate — a clinically approved, lipid-lowering drug that is used to treat cholesterol — improved the blood-brain barrier, cognition, as well as social behaviors in an animal model of 22q.
Why It Matters
The CHOP-Penn research team's findings suggest that mitochondrial dysfunction in the blood-brain barrier influences its integrity and contributes to neuropsychiatric disorders in 22q. Targeting the mitochondria with bezafibrate — as well as other medications that enhance mitochondrial function, or even diet and exercise — could improve or prevent these conditions, according to the researchers.
The blood-brain barrier is a tightly locked layer of endothelial cells that protects the brain from toxins and pathogens circulating in the blood. Deficits in the blood-brain barrier are believed to contribute to conditions ranging from neurodevelopmental disorders, such as autism and schizophrenia, to neurodegenerative conditions, including Alzheimer's and Parkinson's diseases.
22q, also called DiGeorge syndrome, is caused by a chromosomal deletion that includes six mitochondrial genes. It can lead to intellectual disabilities, social challenges, and attention difficulties. An estimated 25% of patients develop schizophrenia, making 22q11.2 deletion one of the strongest risk mutations for the psychiatric disorder.
Having previously discovered that 22q11.2 deletion is associated with both blood-brain barrier and mitochondrial deficits, the CHOP-Penn research team wanted to determine whether these deficits could be related, since mitochondrial deficits can be targeted with medications. Bezafibrate is a PPAR agonist, and this class of drugs has shown positive outcomes in preclinical studies of blood-brain barrier-associated neurological diseases, including stroke, epilepsy, schizophrenia, and Alzheimer's disease.
Who Conducted the Study
Stewart A. Anderson, MD, Associate Chair for Research in the Department of Child and Adolescent Psychiatry and Behavioral Sciences at CHOP and Associate Director of the CHOP/Penn Lifespan Brain Institute, and Jorge Iván Alvarez, PhD, an Associate Professor of Pathobiology at Penn Vet, were the study's co-corresponding authors.
CHOP has the world's largest clinic dedicated to the care of children, adolescents, and some adults with 22q, and a dedicated team of researchers at Penn and CHOP studies the condition as a window into many other diseases.
How They Did It
The researchers investigated mitochondrial function in both animal and human stem cell models of 22q. After identifying a mitochondrial deficit in the models, the researchers hypothesized that treatment with bezafibrate would increase respiration and improve function in the blood-brain barrier. The team treated the models with bezafibrate and measured respiration and barrier integrity, as well as social preferences and recall, to test their hypothesis.
Quick Thoughts
"To our knowledge, a link between PPAR agonists and blood-brain barrier integrity had not been demonstrated previously," Dr. Anderson said. "Since the blood-brain barrier is relatively easily targeted with therapeutics and improvement of the blood brain barrier function improved cognition in our model of 22q, our results could have broad therapeutic implications within the context of 22q and beyond."
What's Next
The researchers hypothesize that the findings may have implications for the targetable role of mitochondrial dysfunction in the blood-brain barrier in other neuropsychiatric conditions, and they plan to study whether they can extend their results beyond the context of 22q.
Where The Study Was Published
The findings were published in the journal Science Translational Medicine. Read more in this CHOP press release.


