HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
CHOP Researchers Pursue the Basic Mechanisms of Genetic Childhood Epilepsies
shafere1 [at] chop.edu (By Emily Shafer)
Ethan Goldberg makes strides in his research on ion channels, genes, and epilepsy.
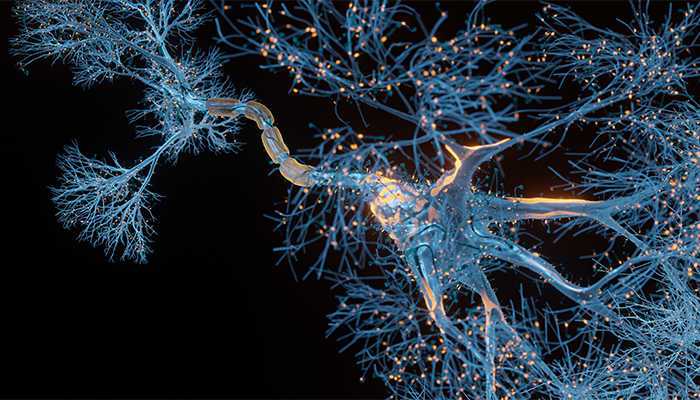
Ion channels are like holes that allow charged particles to pass in and out of neurons. These ion channels, which include sodium, calcium, and potassium channels, are responsible for the brain’s action potentials — discharges of electrical activity in the neurons that mediate all the thoughts, sensations, and actions produced by the brain. When ion channels become impaired, disorders like epilepsy are the result.
Ethan Goldberg, MD, PhD, who is director of the Epilepsy Neurogenetics Initiative (ENGIN), a Frontier Program at Children’s Hospital of Philadelphia, utilizes his expertise in ion channel physiology to seek out novel therapeutics for children with epilepsy and complex neurodevelopmental disorders. His latest research reframes knowledge about the role of sodium channel impairment in Dravet syndrome, and he is launching a new project to study the role of potassium channel impairment in progressive myoclonus epilepsy type 7.
The 2021 recipient of the Fritz E. Dreifuss Award from the American Epilepsy Society, Dr. Goldberg is dedicated to identifying the mechanisms whereby genetic variation leads to epilepsy. He has been studying the mechanistic basis of Dravet syndrome, an epileptic encephalopathy, for the last few years, and is currently working to identify a similar link in progressive myoclonus epilepsy.
“In at least half of children with epilepsy, there is a strong genetic component, and we try to model that in the lab,” Dr. Goldberg said. “The idea is that rather than simply trying an off-the-shelf medication, we can use a patient’s genetics to design a treatment that is targeted toward the underlying cause of their disease.”
Sodium Channels in Dravet Syndrome
Dravet syndrome affects about one in 14,000 live births. It is the most common of the epileptic encephalopathies, which are the most severe type of epilepsy, and which starts in the first year of life, is treatment-resistant, and is associated with moderate-to-severe or profound developmental delay, intellectual impairment, and autism spectrum disorder.
Previous research showed that variants in the gene SCN1A encoding the sodium channel subunit Nav1.1 are the cause of Dravet syndrome. Nav1.1 is preferentially expressed on a subset of interneurons marked by parvalbumin, a calcium-binding protein found in some GABAergic interneurons, which are important for suppressing seizures under normal conditions. Prior work from the Goldberg Laboratory confirmed that these interneurons were dysfunctional early in the disease course, but eventually correct themselves during the chronic phase, in an animal model of Dravet syndrome.
The researchers now reframe this knowledge in a recent publication in Cell Reports. Dr. Goldberg and his team found that while the parvalbumin interneurons do, indeed, recover their normal electrical activity, these electrical discharges — the action potentials — do not propagate down the interneuron axon to the synapse.
“Although these interneurons have recovered their ability to fire electrical discharges for that to have any impact, the charge needs to travel down the nerve axon to the synapse and release the neurotransmitter GABA to other cells,” said Dr. Goldberg, who is also an associate professor of Neurology, Neuroscience, and Pediatrics at the Perelman School of Medicine at the University of Pennsylvania. “We found that the signal wasn’t propagating down to the synapse to impact other cells downstream, redefining our understanding of the pathological mechanism of Dravet syndrome.”
Potassium Channels in EPM7
Dr. Goldberg’s investigation into the role of ion channels in epileptic diseases encompasses another epilepsy type: progressive myoclonus epilepsy type 7 (EPM7). EPM7 is a rare form of epilepsy that starts in childhood with a tremor, and it eventually leaves individuals wheelchair-bound and dependent on others for self-care. Mutations in the KCNC1 gene is a cause of EPM7. The KCNC1 gene encodes the potassium ion channel Kv3.1 and has been a large focus of Dr. Goldberg’s research.
With a new grant from the National Institute of Neurological Disorders and Stroke, Dr. Goldberg and his team seek to further elucidate the role of the KCNC1 mutations on function of the potassium channel Kv3.1 and evaluate a potential treatment. The first aim of the grant is to determine the impact of KCNC1 mutations on Kv3.1 and map out a clinical-genetic-physiological landscape of neurological disorders related to the gene.
The second aim of the grant is to determine the cellular/synaptic basis of the neurological dysfunction of the KCNC1 variant involved in EPM7 in an animal model. This variant impairs function of the Kv3.1 potassium channel. The third aim is to assess a novel agent to repair and activate the Kv3.1 potassium channel, and potentially treat patients with EPM7.
“There are 15 different genetic causes of progressive myoclonus epilepsy, but they all resemble one another and are all currently untreatable,” Dr. Goldberg said. “It is possible that some of the insight we gain as to the mechanisms of this EPM7 subtype could be generalized to the other subtypes of progressive myoclonus epilepsy.”
The Goldberg Lab uses the results of clinical genetic testing towards improved understanding and the development of novel treatments for pediatric epilepsy in preclinical models that will one day improve the lives of children and their families living with epilepsy.