HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
Pennsylvania Pediatric Medical Device Consortium
The Pennsylvania Pediatric Medical Device Consortium (PPDC), formerly the Philadelphia Pediatric Medical Device Consortium, is a collaboration sponsored by the Food and Drug Administration. The PPDC connects Children's Hospital of Philadelphia with the McGowan Institute for Regenerative Medicine and sciVelo, both based at the University of Pittsburgh.
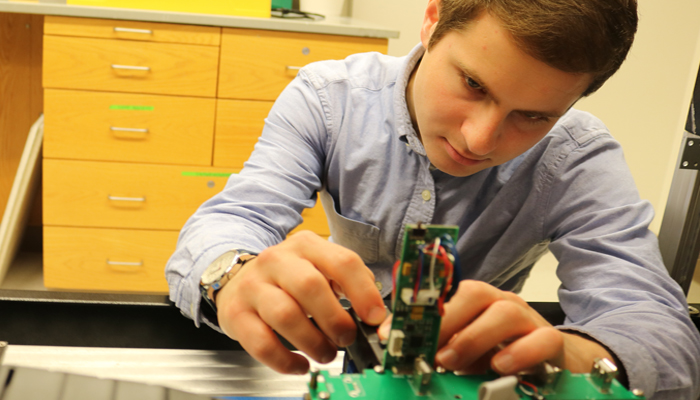
Since its founding in 2013, the PPDC has provided both guidance and seed funding for a range of pediatric products, including an airway clearance system, a powered arm brace, a speech-generating communication system, a vision acuity test for preverbal children, and a portable phototherapy device for newborns with neonatal jaundice. It has assisted more than 250 innovative projects and has awarded 35 seed grants of up to $50,000 each to companies in Pennsylvania and beyond.
In addition to the annual round of seed grants, the PPDC accepts applications at all times for in-kind services and expert advice. Learn more about some projects that PPDC seed grants helped to develop.

The PMD Launchpad is the official home page of the PPDC and hosts both membership materials and funding applications: https://pmdlaunchpad.org/