HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
In This Section
New Kind of CAR T-Cell Changes Scientists’ Approach to Solid Tumors
PC-CARS are a new class of engineered T cells that open the door to treating a wider range of cancers via immunotherapy.
limjr [at] chop.edu (By Jillian Rose Lim)
A powerful new class of engineered T cells are opening the door to treating a wider range of cancers in a wider population of patients through immunotherapy. Meet the peptide-centric chimeric antigen receptor T cell, or “PC-CAR”: Born out of a multi-omics approach and genetic engineering by Children’s Hospital of Philadelphia researchers, the breakthrough therapy is a turning point for treating solid tumors like neuroblastoma, one of the most aggressive pediatric cancers.
In Nature, its developers, John Maris, MD, a lifelong neuroblastoma physician-scientist, and Mark Yarmarkovich, PhD, investigator in the Maris Lab, successfully showed that PC-CARS not only targeted previously unreachable proteins inside cancer cells, but also led to the complete elimination of neuroblastoma tumors in an animal model.
“This research opens up the possibility to target very specific tumor molecules in larger patient populations and truly build toward a personalized approach for treating potentially all cancers,” Dr. Yarmarkovich said. “By using a multi-omics approach, we were able to identify peptides specific to neuroblastoma tumors, but this method could be used in any cancer, substantially broadening the landscape of actionable tumor targets.”
Optimizing Immunotherapy for Solid Tumors
In the last decade, researchers have had tremendous success treating leukemia via CAR T cell-based immunotherapy, wherein the body’s natural defenses are boosted to destroy cancer cells. The majority of childhood solid cancers, however, do not have the same track record for effectiveness. While engineered T cells can identify targets on the surface of cells in leukemia, most solid tumors harbor the proteins driving cancer inside the nuclei of their cells.
Nevertheless, Dr. Yarmarkovich had an idea. Fragments of proteins can present on a cell’s surface to the immune system as peptides on the major histocompatibility complex (MHC). With this in mind, what if the team developed a synthetic CAR with the ability to recognize and target the peptides on the cell surface that were tumor-specific?
The idea had its hurdles: First, the synthetic CAR would need to be able to differentiate tumor-specific peptides from those existing in normal tissues as well as similar-looking peptides. This was key for avoiding cross-reactivity and lethal toxicity.
Thus, Drs. Yarmarkovich and Maris began with a multi-omics approach to target discovery, combining their analyses from different omics data sets, including genomics and immunopeptidomics.
Picking Through the Peptides: a Multi-Omics Approach
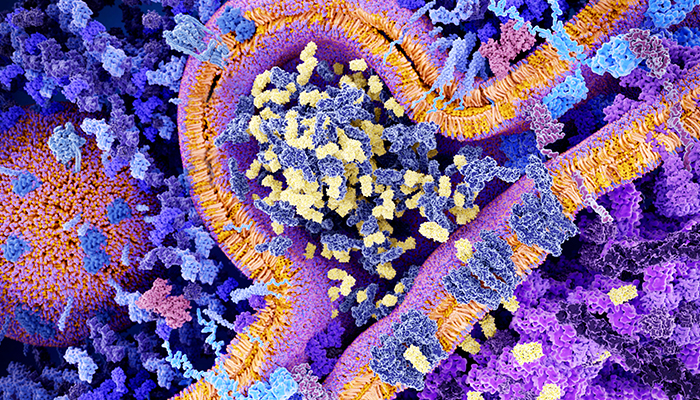
The team first looked empirically at the type and number of peptides presented on MHC molecules taken from neuroblastoma cells. Next, they utilized a large genomic dataset to identify which peptides were unique to neuroblastoma and not expressed by normal tissues. Those peptides derived from genes essential to the tumor, such as PHOX2B, and those with characteristics required to engage the immune system ranked high on their list. The team then filtered the remaining tumor peptides against a database of MHC peptides on normal tissues, removing any peptide with a parent gene represented in normal tissue.
“Any one omics data set alone wouldn't have gotten us there,” Dr. Yarmarkovich said. “But by being able to integrate them, that’s really what got us to the tumor specificity.”
Spotlight on PHOX2B: Developing the PC-CAR
For this particular study, the researchers focused on one particular peptide derived from a gene, PHOX2B, that Dr. Maris’ lab had identified as the first hereditary neuroblastoma gene 20 years ago. They developed a PC-CAR that could not only recognize this tumor-specific peptide but could do so in different HLA types – meaning that it could be applied to patients of diverse genetic lineages.
“Dr. Yarmarkovich shows in his paper that PC-CAR recognizes several other HLA types, including one that is the most common one in people of African descent,” Dr. Maris said. “So, the next step for neuroblastoma is to build out a warehouse of four or five of these to cover any potential patients.”
The approach can be applicable to any cancer, according to Drs. Maris and Yarmarkovich, Though they focused on PHOX2B due to its association with neuroblastoma, other scientists may seek to use the approach with other genes in association with other cancers.
“We’ve made all our data public,” Dr. Maris said. “We can't focus on all of the peptides we discovered in neuroblastoma, so [scientists are] welcome to pick their favorite peptides. Another scientist out there might have a gene of interest that we just didn't focus on that they might want to take to a PC-CAR. So, we’re very hopeful that that this will open up this class of drugs, these PC-CARs, as a new modality.”
Next Steps in Neuroblastoma Research
In the next two years, Drs. Maris and Yarmarkovich will bring their PHOX2B PC-CAR to neuroblastoma patients through a clinical trial with support from a Cell and Gene Therapy Collaborative Acceleration grant.
Dr. Maris is particularly excited by the prospect of PC-CARS as a new approach to the “explosively aggressive” cancer. Currently, the only way clinicians can approach the metastases of neuroblastoma is via standard chemotherapy, which has its challenges. While cancer cells become more susceptible to chemotherapy the quicker they divide, they also become more prone to develop new mutations that can evade the treatment. Thus, neuroblastoma patients can respond to chemotherapy but ultimately relapse.
“I have watched many neuroblastoma patients die because of a lack of effective therapies, and this research is exciting because it is potentially a new curative drug – and not just for neuroblastoma,” Dr. Maris said. “We’re sold on the power of this approach for other cancers. Clearly, immunotherapy is an underutilized for a lot of important reasons and this approach will obviate some of the main obstacles to its success.”