HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
Improving Health With Research That Spans a Lifetime
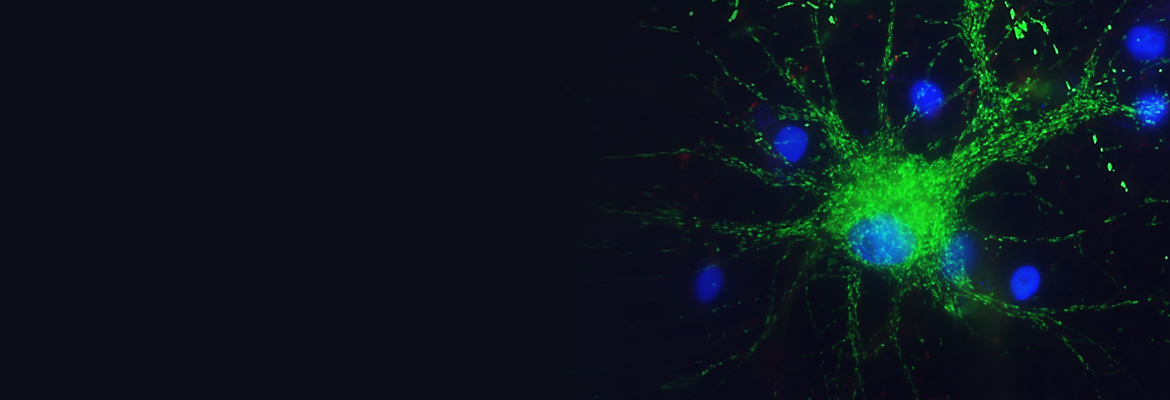
Benchmarking Brain Development
"Our work brings together a huge amount of imaging data that will continue to grow, allowing researchers and eventually clinicians to evaluate brain development against standardized measures."
Researchers at Children’s Hospital of Philadelphia Lifespan Brain Institute, the University of Pennsylvania, and University of Cambridge, have developed a new tool called BrainChart that uses magnetic resonance imaging (MRI) data to provide benchmarks of brain development over the human lifespan. Described in Nature, this interactive open resource harmonizes brain images in a way that allows researchers to measure brain development against reference charts, like those used for evaluating children’s height and weight.
“There are no standardized growth charts for brain development like there are for other growth metrics such as height and weight, despite the fact that we know the brain goes through many changes over the human lifespan,” said Aaron Alexander-Bloch, MD, PhD, director of the Brain-Gene-Development Lab within the Department of Child and Adolescent Psychiatry and Behavioral Sciences at CHOP. “Our work brings together a huge amount of imaging data that will continue to grow, allowing researchers and eventually clinicians to evaluate brain development against standardized measures.”
30 Year Anniversary Milestone
"The creation of the Center allowed us to start to shine a light on this group of brain-based disorders that require all of these disciplines to work collaboratively."
In 2022, the multidisciplinary team at the Intellectual and Developmental Disability Research Center (IDDRC) celebrated 30 years of continuous funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).
Michael Robinson, PhD, co-leads the IDDRC at Children’s Hospital of Philadelphia and the University of Pennsylvania, a nucleus for IDD research that serves as the foundation for collaboration, alongside Robert Schultz, PhD, director of the Center for Autism Research. For three decades, the IDDRC has provided what Dr. Robinson calls “the glue” uniting scientists across different disciplines. Working with researchers in genetics, developmental and behavioral pediatrics, neurology, psychiatry, biostatistics, and more, the IDDRC enables cutting-edge IDD research by bringing the brightest scientific minds together with the latest innovations.
“Thirty years prior, there wasn’t a structure to support collaboration between various disciplines,” Dr. Robinson said. “The creation of the Center allowed us to start to shine a light on this group of brain-based disorders that require all of these disciplines to work collaboratively. We all know somebody, or know of somebody, who has one of these disorders, and the IDDRC exists to bring researchers to work together because they can learn from one another.”
Diagnosing Leigh Syndrome
"This study demonstrates that Leigh syndrome disorders should be considered a diagnostic possibility at the time when a child is recognized to have early developmental delays ..."
Leigh Syndrome is characterized by neurodevelopmental regression, where a child loses previously achieved skills as metabolic strokes occur in their deep brain regions. But new research from the Mitochondrial Medicine Frontier Program at Children’s Hospital of Philadelphia suggests that developmental delays associated with Leigh syndrome, the most common pediatric mitochondrial disorder, may occur earlier than regression and metabolic stroke, which could provide clinicians with an opportunity for earlier diagnosis and therapeutic interventions.. The journal Molecular Genetics and Metabolism published the study findings.
“This study demonstrates that Leigh syndrome disorders should be considered a diagnostic possibility at the time when a child is recognized to have early developmental delays, even if the child hasn’t yet had a serious regression episode that is often the trigger to begin the diagnostic process,” said clinical geneticist Marni Falk, MD, executive director of the Mitochondrial Medicine Frontier Program.
Cyberbullying and Suicidality
"At a time when young adolescents are spending more time online than ever before, this study underscores the negative impact that bullying in the virtual space can have on its targets."
Researchers from the Lifespan Brain Institute (LiBI) of Children’s Hospital of Philadelphia and the University of Pennsylvania published findings in JAMA Network Open that revealed adolescents who are targets of cyberbullying are more likely to report suicidal thoughts and attempts — an association that goes beyond the link between suicidality and traditional offline bullying — and supports the concept that cyberbullying is a distinct phenomenon.
“At a time when young adolescents are spending more time online than ever before, this study underscores the negative impact that bullying in the virtual space can have on its targets,” said Ran Barzilay, MD, PhD, assistant professor at LiBI and an attending psychiatrist at CHOP. “Given these results, it may be prudent for primary care providers to screen for cyberbullying routinely in the same way that they might screen for other suicide risk factors like depression. Educators and parents should also be aware of the substantial stress bullying in the cyberworld places on young adolescents.”
Role of Bioenergetics
"Recognizing the role of mitochondrial dysfunction in neuropsychiatric disorders may lead to the development of better diagnostic tools as well as targeted treatments for patients with 22q-associated schizophrenia."
Researchers from Children’s Hospital of Philadelphia and the University of Pennsylvania showed how the “batteries” of cells, or mitochondria, are highly implicated in whether patients with the chromosome 22q11.2 deletion syndrome develop schizophrenia. The results of the study may eventually lead to targeted prevention and treatment strategies for patients with the condition. The findings appeared in JAMA Psychiatry.
The team of researchers showed that mitochondrial function was affected in patients with 22q and a schizophrenia diagnosis, with reduced levels of ATP, a major energy source for cells produced largely by mitochondria. However, ATP levels were not reduced in patients with 22q who were not diagnosed with schizophrenia. In fact, the expression of multiple genes encoding for oxidative phosphorylation, a process that helps produce ATP, was upregulated compared with both the 22q and schizophrenia group and the control group. These findings suggest that increased mitochondrial biogenesis is associated with the absence of schizophrenia in 22q.
“Bioenergetics and mitochondria have historically not been thought to play a significant role in autism spectrum disorders and schizophrenia,” said Douglas Wallace, PhD, director of the Center for Mitochondrial and Epigenomic Medicine, “but our findings from this study coupled with previous findings show that mitochondrial dysfunction may play an important role in these neuropsychiatric disorders. Recognizing the role of mitochondrial dysfunction in neuropsychiatric disorders may lead to the development of better diagnostic tools as well as targeted treatments for patients with 22q-associated schizophrenia.”
Long-term Picture
"That longitudinal aspect is relatively rare, and so this gives us tremendous opportunity to study typical and atypical neurodevelopment."
As part of the multi-site HEALthy Brain and Child Development Study (HBCD), Children’s Hospital of Philadelphia researchers are building a comprehensive, long-term picture of healthy neurodevelopment through the power of big data collected in extraordinary detail. The HBCD follows 7,500 mothers and their children from 24 locations across the United States from before birth to 10 years of age to better understand which harmful and protective environments exert the greatest impact on child development. This study will help to improve the health and development of children across the nation.
Leading the multidisciplinary team, are CHOP investigators Hao Huang, PhD, of the Department of Radiology and Sara DeMauro, MD, MSCE, of the Division of Neonatology. The researchers, including collaborators from the University of Pennsylvania, are collecting a multimodal data set from hundreds of babies over the course of a decade in an unparalleled landmark study.
“This is a very big longitudinal follow-up,” Dr. Huang said. “It’s very difficult to pull data from the second trimester in utero all the way to adolescence, while also including the mother’s data. That longitudinal aspect is relatively rare, and so this gives us tremendous opportunity to study typical and atypical neurodevelopment.”