HOW CAN WE HELP YOU? Call 1-800-TRY-CHOP
Curiosity and Technology Help to Find Drivers of Rare and Complex Diseases
New Immunodeficiency Disease
Researchers at CHOP discovered a new immunodeficiency disease, which they named PU.1 Mutated Agammaglobulinemia (PU.MA), that prevents the formation of infection-fighting B cells and antibodies. They performed whole exome sequencing on 30 patients born without B lymphocytes and discovered that six patients had a mutation in the SPI1 gene. This gene encodes the PU.1 protein, and because of the mutation, there was less PU.1, and B cells were unable to form. The findings appeared in the Journal of Experimental Medicine.
The paper’s senior author, Neil Romberg, MD, investigator in the Department of Pediatrics, and the first author, Carole Le Coz, PhD, collaborated with numerous CHOP departments, including the Roberts Individualized Medical Genetics Center, the Center for Spatial and Functional Genomics, and the Cancer Center, as well as institutions worldwide.
“Identifying rare genetic variants in patients is now faster, cheaper, and more readily available using next-generation sequencing,” Dr. Romberg said. “Proving variant causality still requires multiple orthogonal scientific approaches and big collaborative teams that ideally include patients/patient families.”
Full Phenotypic Landscape
CHOP researchers affiliated with the Epilepsy Neurogenetics Initiative (ENGIN) compiled a genetic and clinical analysis of more than 400 individuals with SCN2A-related disorder, which is linked to various neurodevelopmental disorders, including epilepsy and autism. Linking the clinical features to genetic abnormalities in a standardized format may help improve identification of the disorder and clinical intervention.
Researchers led by Ingo Helbig, MD, director of the genomic and data science core of ENGIN, used Human Phenotype Ontology (HPO), a method that standardizes patients clinical features and allows that data to be translated like genetic data. They extracted phenotypic information from SCN2A-related disorders published over nearly two decades. Across 413 unrelated individuals, the study team derived more than 10,000 clinical annotations in HPO terms, with a total of 562 unique terms, allowing the researchers to link clinical features with specific gene variants. The findings appeared in Genetics in Medicine.
“This work, built upon our previous studies, now provides a framework on how HPO terminology can map complex clinical data in a variety of rare disorders to get to answers about clinical features, natural history, and outcomes that we do not have yet,” Dr. Helbig said.
Novel Mechanistic Link
Researchers in the CHOP Cancer Center discovered that the oncogene meningioma-1 (MN1) is linked to acute myeloid leukemia (AML) through its effect on the BAF complex, a site crucial for the regulation and differentiation that is mutated in about 20 percent of cancers. They found that overexpression of MN1 strengthens the BAF complex’s interaction with DNA, which has consequences on blood cell production.
In addition, researchers found that MN1’s ability to stabilize the BAF complex is dependent on an MN1 protein structure called the polyQ-stretch. PolyQ-stretches are best known for their role in neurodegenerative diseases. Researchers found that deleting the polyQ-stretch impairs MN1’s ability to over-stabilize the BAF complex binding to DNA, thus allowing blood cells to differentiate normally. The study appears in Molecular Cell.
“What’s exciting about this research is its potentially broad implications,” said Kathrin Bernt, MD, a physician-scientist in the Leukemia and Lymphoma Program, and senior author of the paper. “This is a look at how cancer can happen beyond the classic mechanisms of overactive signaling and DNA damage.”
SMARCA5 Variants Associated with Developmental Changes
Researchers in the Center for Applied Genomics (CAG) identified how variants of a gene responsible for packing and condensing genetic material cause certain neurodevelopmental disorders . The gene, SMARCA5, is responsible for encoding a chromatin remodeling complex. Preclinical evidence suggests that variants of this gene were associated with developmental changes, but a specific disorder was never described.
The study, which appeared in Science Advances, reports on 12 patients across 10 unrelated families. The patients had similar clinical features, including mild developmental delay, short stature, and microcephaly.
“Our study is the first to describe how certain germline mutations in SMARCA5 are responsible for a spectrum of neurodevelopmental delays,” said study leader Dong Li, PhD, a research scientist in CAG. “Apart from identifying patients with such germline variants for the first time, our extended translational modeling study efforts to determine the underlying functions for these variants further elucidated their clinical relevance.”
Dr. Li collaborated with Yuanquan Song, PhD, of the Department of Pathology and Laboratory Medicine at CHOP. Hakon Hakonarson, MD, PhD, director of CAG, was the senior author of the study.
Paving the way for Potential Therapies
Researchers led by Wei Tong, PhD, investigator in the Division of Hematology at CHOP, identified a protein coding gene, HectD1, that appears to be responsible for hematopoietic stem cell (HSC) regeneration via ribosome assembly. The discovery paves the way for potential therapies for children with ribosomopathies, a group of inherited bone marrow failure disorders that result from impaired ribosome function.
The findings, which appear in Cell Stem Cell, found that the ribosomal assembly factor ZNF622 mediates the function of the E3 ubiquitin ligase HectD1 in HSC regeneration. Knocking out the Znf622 gene in HSCs that lack the HectD1 gene restores protein synthesis and HSC production.
“These findings not only highlight the connection between protein degradation, ribosome assembly, and stem cell production, but they also reveal the potential for knocking down Znf622 to restore proper bone marrow function, which is critical for child development,” Dr. Tong said. “Future research should look at this mechanism as a potential target for patients with these disorders.”
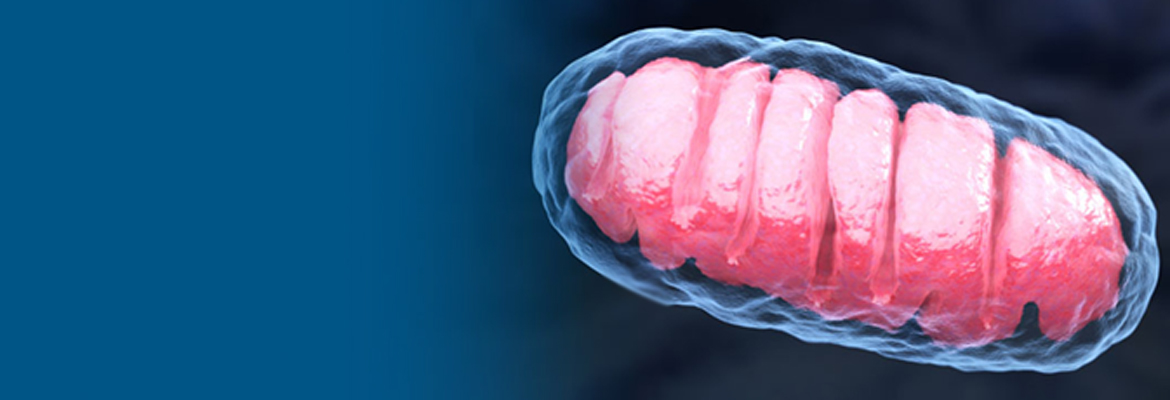
Yin and Yang: Mitochondrial Disease vs Cancer
The Mitochondrial Medicine Frontier Program and the Center for Data-Driven Discovery in Biomedicine (D3b) at CHOP joined forces to form the Mitochondria and Cancer Connections (MC2) Research Program. Under the new program, researchers led by Marni Falk, MD, director of the Mitochondrial Medicine Frontier Program, and Adam Resnick, PhD, director of D3b, aim to leverage their existing centers and knowledge to establish a research initiative to find new insight into disease processes and therapeutics, at the intersection of mitochondrial disease and cancer. They will harness a data analysis and sharing platform developed by D3b called CAVATICA to analyze multi-omics data.
“Ultimately, we aim to steal strategies from cancer to help mitochondrial disease cells grow and function better, while at the same time stealing strategies from mitochondrial disease to slow down cancer,” Dr. Falk said. “In other words, our basic goal is to learn from the survival strengths and weaknesses of one disease, to shed light on precision treatment strategies for the other. If we’re lucky, we’ll find therapies for both classes of diseases.”